Respiratory diseases, including pneumonia, cause around one million deaths in Europe each year. The disease is very dangerous, especially for the elderly and those with chronic illnesses, and one of the most common causes of pneumonia is bacterial infections caused by pneumococci, among others.
12 November is World Pneumonia Day to draw attention to this forgotten and underestimated disease. This is important especially during the coronavirus pandemic, when we should prevent pneumonia even more than usual.
As many as 450 million people worldwide contract pneumonia each year, and four million of them die. Among Poles, 100 000 people fall ill in a year. These are official figures. There are probably twice as many pneumonia cases in Poland, because some are not hospitalised and not registered - says Prof. Adam Antczak from the Department of General and Oncological Pulmonology, Medical University of Lodz. Figures from two years ago (the latest) show that as many as 18,500 Poles died of pneumonia during the year - adds Professor Adam Antczak
Inflammation lungs. Pneumonia is a disease that attacks the alveoli in the lungs. It can be caused by viruses, fungi and bacteria, among others. The predominant symptoms include cough (with expectorated secretions), fever, chills, chest pain, more frequent and difficult breathing. This is not just a more severe cold. The disease, particularly in the elderly, is associated with a high risk of complications and death - the underlines Prof. Adam Antczak
People over 65 years of age and chronically ill adults with co-morbid health problems and young children are most commonly affected by pneumonia. Lung diseases, especially COPD, heart disease, liver disease, kidney disease, nephrotic syndrome, diabetes mellitus, cancer and all immunocompromised conditions regardless of their cause, favour the development and severity of the disease.
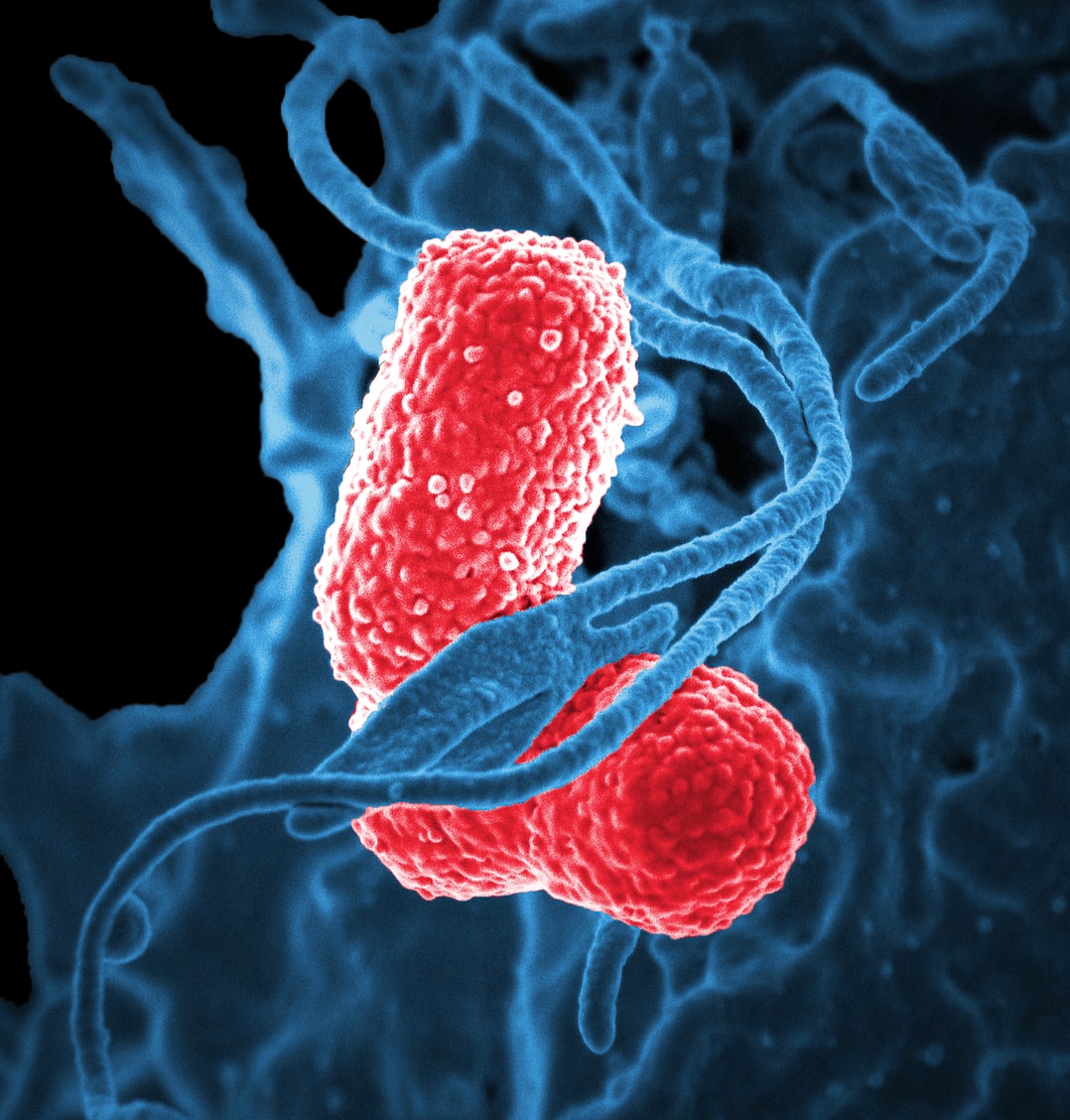
Pneumococcal pneumonia. The bacteria that most commonly cause pneumonia in adults are pneumococci.[1] In older adults and in adults with chronic diseases and immune disorders, they can lead to hospitalisation, exacerbation of concomitant diseases and, in some cases, death.
Pneumonia accounts for approximately 50% of hospitalisations for respiratory diseases in adults in Poland.[2] In 2019, nearly 60,000 adults were hospitalised for pneumonia.[3] When contracting pneumococcal pneumonia, 1 in 20 people may die, but the rate may be higher among older people[4] It is estimated that in 2013. 1 in 5 deaths among adults due to lower respiratory tract infections was related to pneumococcal pneumonia. [5]
Pneumonia and coronavirus. Even before the pandemic, pneumonia cases in seniors and adults with chronic diseases and immune disorders often led to hospitalisation and exacerbation of concomitant diseases and even death. 8
In addition, during a pandemic, the risk of hospitalisation should be minimised because of the risk of COVID-19 infection. Flu symptoms often resemble those of COVID-19, which may expose the patient to unnecessary contact with a facility for COVID-19-infected patients. The viral infection may open the way for bacteria and contribute to the development of pneumonia, for example. The elderly, who in addition have chronic illnesses, are always at the highest risk of such a complication. Recent/existing studies indicate that pneumococci can cause co-infection in COVID-19.[6]
Treatment of pneumococcal pneumonia. Pneumococcal pneumonia is treated with antibiotics. However, treatment is also not facilitated by the fact that pneumococcal bacteria are resistant to antibiotics and infections caused by them simply heal poorly. 9 – Treatment of pneumococcal infections is not straightforward. Often hospitalisation is required, which in the era of SARS-CoV-2 is fraught with additional risks. In the course of pneumococcal pneumonia, the chronic disease from which the patient suffers may be exacerbated. A vicious circle is created, because pneumococcal pneumonia exacerbates chronic diseases, and this makes the treatment of pneumonia more difficult – says Professor Aneta Nitsch-Osuch.
Therefore, during a pandemic, we especially need to protect ourselves not only from coronavirus infection, but also from contracting pneumonia. - Co-infections are more severe, so the situation of a person who has both pneumonia and becomes infected with coronavirus is definitely worse. And in patients with COVID-19, it is pneumococci that are most often detected at the same time – says Professor Adam Antczak.
How to protect yourself against pneumococcal pneumonia? Not everyone is at the same risk of pnemococcal infection including pneumococcal pneumonia. Factors that increase the risk of pneumococcal disease in adults can be divided into four categories:
- Age - Over the age of 50, we are at greater risk of disease,
- Immune disorders - Congenital and acquired immune disorders, HIV infection, chronic kidney disease, nephrotic syndrome, leukaemia, Hodgkin's lymphoma, non-Hodgkin's lymphomas, immunosuppression, uogóflaxseed cancer,
- Diseases chronic - chronic heart disease, chronic lung disease (including asthma), diabetes, chronic liver disease including cirrhosis, sickle cell anaemia, cerebrospinal fluid leakage, cochlear implant, congenital and acquired asplenia,
- Unhealthy behaviour - smoking and alcohol abuse. [7]
People with influenza are also at risk of pneumococcal infection. Streptococcus pneumoniae is one of the most common pathogens detected in patients hospitalised for influenza.[8] Severe influenza can favour the development of pneumococcal pneumonia. Up to 35% cases of hospitalisation due to influenza lead to concomitant bacterial infection S. pneumoniae. Meanwhile, post-influenza bacterial pneumonia is a major cause of morbidity and mortality during an influenza epidemic/pandemic.[9]
As with children, the recommended form of prevention of infection with the dangerous bacterium is vaccination. Effective vaccinations are available for adults to protect against Invasive Pneumococcal Disease and pneumococcal pneumonia. The older type polysaccharide vaccine requires repeated inoculations, the conjugated vaccine requires only one administration. It is worth mentioning that the pneumococcal vaccine can be given together with the influenza vaccine.
[1] Jansen AG, et al. Clin Infect Dis. 2009;49(2):e23-e29.
Reproduced from [Welte T et al, Thorax, volume 67(1), pages 71-79, 2012] with permission from BMJ Publishing Group Ltd. 2 Lode HM. Respir Med. 2007;101(9):1864-1873
[2] Data prepared as part of the project entitled: Health Needs Maps - System Analysis and Implementation Database, Ministry of Health 2019_ http://www.mpz.mz.gov.pl.
[3] Data prepared as part of the project entitled: Health Needs Maps - System Analysis and Implementation Database, Ministry of Health 2019_. http://www.mpz.mz.gov.pl.
[4] Centers for Disease Control and Prevention. Pneumococcal Disease. https://www.cdc.gov/pneumococcal/about/index.html (accessed August 2020).
[5] Naghavi M, Wang H, Lozano R et al. GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013.Lancet. 2015; 385(9963):117-171
8 http://koroun.nil.gov.pl/wp-content/uploads/2020/06/Inwazyjna-choroba-pneumokokowa-IChP-w-Polsce-w-2019-roku.pdf
[6] Xiaojuan Zhua et al. Co-infection with respiratory pathogens among COVID-2019 cases. Virus Research 285 (2020) 198005
9http://koroun.edu.pl/dane-epidemiologiczne/
[7] Centers for Disease Control and Prevention. Active Bacterial Core surveillance (ABCs) report. Emerging Infections Program Network: Streptococcus pneumoniae, 2014. http://www.cdc.gov/abcs/reports-findings/survreports/spneu14.pdf. Accessed April 11, 2017. 2. Kobayashi M, et al. MMWR Morb Mortal Wkly Rep. 2015;64(34):944-947. 3. Centers for Disease Control and Prevention. Pneumococcal disease. In: Hamborsky J, Kroger A, Wolfe S, eds. Epidemiology and Prevention of Vaccine-Preventable Diseases. 13th ed. Washington, DC: Public Health Foundation; 2015:279-296.
[8] Based on a systematic review and meta-analysis of 27 studies, published since 1982.
* Additional pathogens detected included H. influenzae (3,8%), K. pneumoniae (2,8%), M. pneumoniae (2.6%), and other (15.3%)
[9] Klein EY, et al. Influenza Other Respir Viruses. 2016;10(5):394-403. 2. Morris DE, et al. Front Microbiol. 2017;8:1041. 3. Gibson G, Loddenkemper R, Sibille Y, Lundback B, eds. European Lung White Book. Sheffield, United Kingdom: European Respiratory Society; 2013. http://www.erswhitebook.org/chapters/. Accessed August 1, 2018.