Patient organisations and experts recommend changes in the psoriasis treatment drug programme.
29 October celebrated World Psoriasis Day, which provided an opportunity for a series of meetings, discussing the current needs of patients struggling with psoriasis. Patients and clinicians highlighted that there have been significant improvements in access to treatment in recent years. Despite this, there are still unmet needs and areas for change/improvement. Small systemic changes could bring huge benefits to psoriasis patients.
Psoriasis is a chronic autoimmune disease
As a chronic systemic inflammatory disease, plaque psoriasis is associated with comorbidities such as psoriatic arthritis, metabolic syndrome, obesity and depression. Importantly, each exacerbation occurring in the course of psoriasis is also associated in patients with worsening comorbidities. Psoriasis therefore has an impact on the whole body. It also has a very negative impact on patients' mental health, as it is a highly stigmatising disease due to the skin lesions and disability that can result from psoriasis. The disease in most patients has a huge impact on all areas of life, from family to work. It is a disease that determines the entire life of the patient. It is therefore important that, in the treatment of psoriasis, doctors have the opportunity to individualise therapy and adapt it to the needs of the individual patient in order to eliminate, as far as possible, the impact of the disease on the patient's life.
Recommendations from clinicians and patient organisations
Psoriasis patients want to function normally in both their personal and professional lives. In order to improve their situation and facilitate their chance of returning to a normal life, it is necessary to focus on freeing them from lesions on the body, which will also affect their mental condition. It is worth remembering that psoriasis is associated with comorbidities. Systemic inflammatory changes also affect patients' quality of life. The earlier effective treatment is initiated, the greater the chance of inhibiting the inflammatory process.
On the occasion of World Psoriasis Day, clinicians and patients discussed the current situation of psoriasis patients in Poland. They emphasised how much had already been achieved, while at the same time pointing to a number of areas which, in their view, are extremely important from the perspective of patient care and whose improvement will have a direct impact on improving the quality of life of psoriasis sufferers in Poland.
They drew attention in particular to:
The need to abolish the mandatory interruption of biologic treatment for psoriasis.
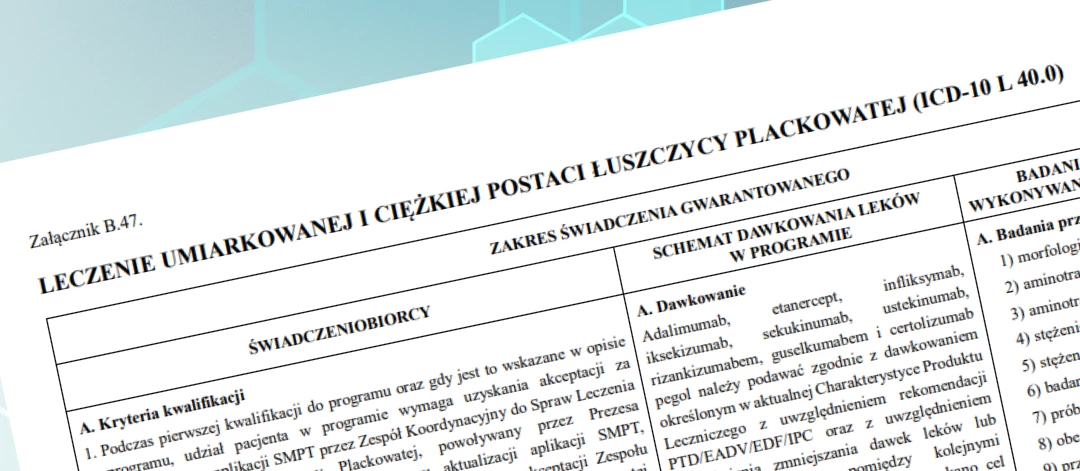
The main demand is abolition recordswhich limit the treatment time for the most seriously ill patients to 96 weekswhich applies to the most modern drugs reimbursed under the drug programme. Currently, after 96 weeks, a psoriasis patient whose lesions regress is discontinued until symptoms worsen and worsen again. The medical and patient communities consider such behaviour unethical and unacceptable - with no medical justification.
For patients, a break in treatment means that symptoms such as pain, itching and burning start to hinder daily activities again. The skin becomes covered with unpleasant and embarrassing lesions that patients do not want to show, thus excluding themselves from social life. This often leads to psychological problems, resulting in the need for therapy or psychiatric treatment. This results in additional costs for the public payer due to sick leave, as well as the treatment of co-morbidities. At the same time, it should be emphasised that the above-mentioned limitation has been lifted in practically all other drug programmes (e.g. in rheumatology, gastroenterology).
Marta (37) says what a break in treatment means to her – You know there is a medicine that works, that will help you. But it's not that simple. To get it you have to fight a really long battle with all the available methods to fight psoriasis, of course it takes time, you suffer, but you see the goal. Finally you reach it, you get that long-awaited drug and ... the worst begins. Why? Because it works, it changes your life. People stop looking at you with disgust, you wear a short-sleeved shirt to the gym again, nothing hurts, nothing itches, you have sex again with the lights on. But you are still accompanied by fear, fear of the passing of time. Because when the 96 weeks are up, they will take away your medicine. Why? [I finished my therapy in November 2022. Today is 10 January 2023, I am sitting in the office in front of my doctor. She says to me that I have to come back when I have 10% body involvement. I guess she can see that I'm wondering how much that is because she says, "you must have psoriasis the size of your hand times 10". I think he's trying to pour some optimism into me because he says it's a less restrictive requirement than it used to be. Really? 10 hands? Ink-black tears are streaming down my cheeks. I no longer have the strength to fight them...*.
Need to increase access to further therapeutic options
Clinicians point to the need to make further therapeutic options available to patients with moderate to severe plaque psoriasis. It is important to point out that patients with psoriasis have different disease courses, vary in their clinical symptoms, not every drug is suitable for every patient, and not every drug will provide the expected results. In addition, the treatment effect of achieving psoriasis-free skin is still not achievable in many patients. An effect that is most desired by both patients and doctors. For this reason, patient organisations and clinicians point to the need for more tools to be introduced/available to best help all patients. It is also important to bear in mind that patients with chronic inflammatory diseases stop responding to a given treatment over time and need to have their therapy changed.
Experts call for the introduction into the drug programme of the latest drug from the interleukin-17 inhibitor group, which has a slightly different mechanism of action than the drugs from this group available on the market so far and which would provide chances for better treatment outcomes/increase the range of possible therapies for patients.
Another recommendation is increasing the number of biological medicineswhich could be treated children. Currently, in the drug programme, young patients only have access to one drug, while adults have the option of being treated with 10 preparations.
Lowering the disease severity criterion for state-of-the-art molecules
Recent studies confirm that starting effective psoriasis treatment as early as possible in the course of the disease allows for better therapeutic outcomes and longer remissions, and thus has a huge impact on the long-term quality of life of psoriasis patients.
As clinicians point out, changing the above four issues would ensure that Polish patients would be treated at the best, world-class level.
World Psoriasis Day was a good opportunity to bring the public closer to the problems that people with psoriasis face on a daily basis. However, the conclusions and experiences developed during the events surrounding World Psoriasis Day are not optimistic. What is still needed is a substantive discussion and the involvement of all stakeholder groups in improving the quality of life of patients with this difficult and extremely stigmatising condition.